Key Takeaways
- California’s homeless crisis is associated with high housing costs, inadequate shelter spaces, deinstitutionalization, and changes in the criminal justice system.
- To improve housing affordability, California needs to streamline and accelerate housing production and reexamine the regulations that have hindered new housing development.
- To reduce the unsheltered homeless population, more shelter capacity and increased investment in cost-effective housing are needed.
- A large share of the chronically homeless suffers from drug addiction and mental health problems. More treatment facilities and lower barriers for treatment are needed.
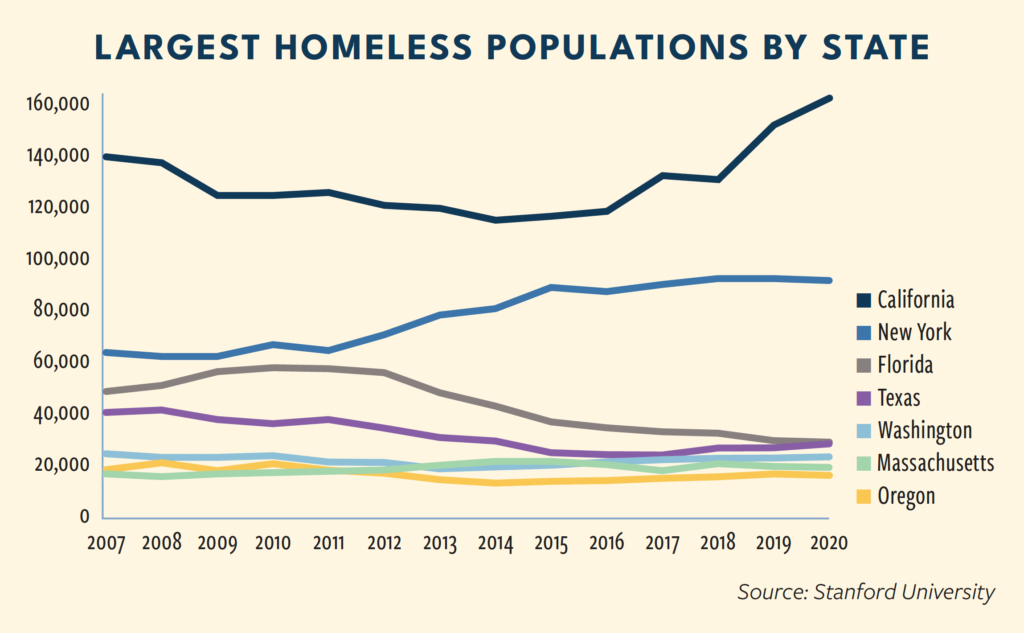
For decades, California has had one of the country’s largest populations of unhoused people. In recent years, however, the challenges have severely worsened for the Golden State. The homelessness counts in California rose by 42 percent between 2014 and 2020, while the rest of the country had a 9 percent decrease. On any given night, the state has more than 160,000 homeless persons.
Figure 1: State Homelessness Point-in-Time Counts
About 70 percent of California’s homeless live outside a shelter system, sleeping in tents, public open spaces, or vehicles. That’s a stark contrast with New York, where only 5 percent of the homeless population are unsheltered. Opinions diverge on how to reduce the unsheltered homeless population. Disputes center around whether to focus on building permanent housing versus shelters and interim housing and the legality of public encampments.
Another challenge lies in the interactions between mental illness, drug addiction, and homelessness. In 2020, about 25 percent of all homeless adults in Los Angeles County had severe mental illnesses such as a psychotic disorder and schizophrenia and 27 percent had a long-term substance use disorder. Moreover, a higher percentage of so-called chronically homeless1 have drug addiction, a severe mental illness, or both.
Meanwhile, state and local governments have spent billions of dollars to combat homelessness. Between 2018 and 2020, California spent $13 billion on homelessness, across nine state agencies through 41 programs (Har 2021). Governor Gavin Newsom signed a $12 billion funding package of bills in 2021 to tackle the homelessness crisis.
With so much money being spent to combat homelessness, what are the prospects for reducing the numbers once and for all? This policy brief provides an overview of the major contributing factors to the rising homelessness in California and highlights the impact of policies, legislation, and regulations on several of those factors: housing, mental health, illicit drug use, and crime.
Housing affordability and availability
California has one of the most expensive and fastest-growing housing markets. Between 2000 and 2021, home values more than tripled in most metro areas in the Golden State. As of March 31, 2021, the typical home value in California was $775,000, double the levels in New York and Florida and triple the level in Texas (Zillow).
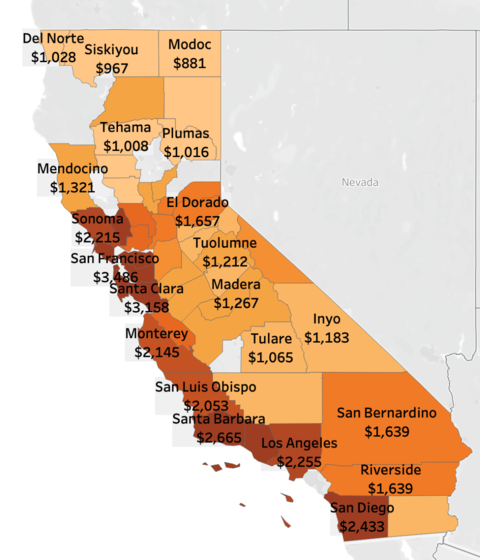
The median rent for a two-bedroom apartment is well over $3,000 in the Bay Area, more than twice as much as the national average of $1,200. In more than two-thirds of California’s ZIP codes, families are “rent-burdened” as they spend more than 30 percent of their income on rent (ABC 2021).
High housing costs and a low stock of affordable housing create a precarious situation, especially for lower-income families and individuals who are at higher risk of becoming homeless.
Figure 2: Median Rent for a Two-Bedroom Apartment, California, 2022
High housing costs are rooted in both demand- and supply-side factors. On the demand side, California boasts robust jobs and household income growth. Between 1990 and 2017, high-paying industries embraced the most vigorous job growth, including information technology (up 127 percent), education and health services (up 107 percent), and professional and business services (up 84 percent) (CA Government 2019). In 2021, the state accounted for 44 percent of the nation’s new jobs that year.
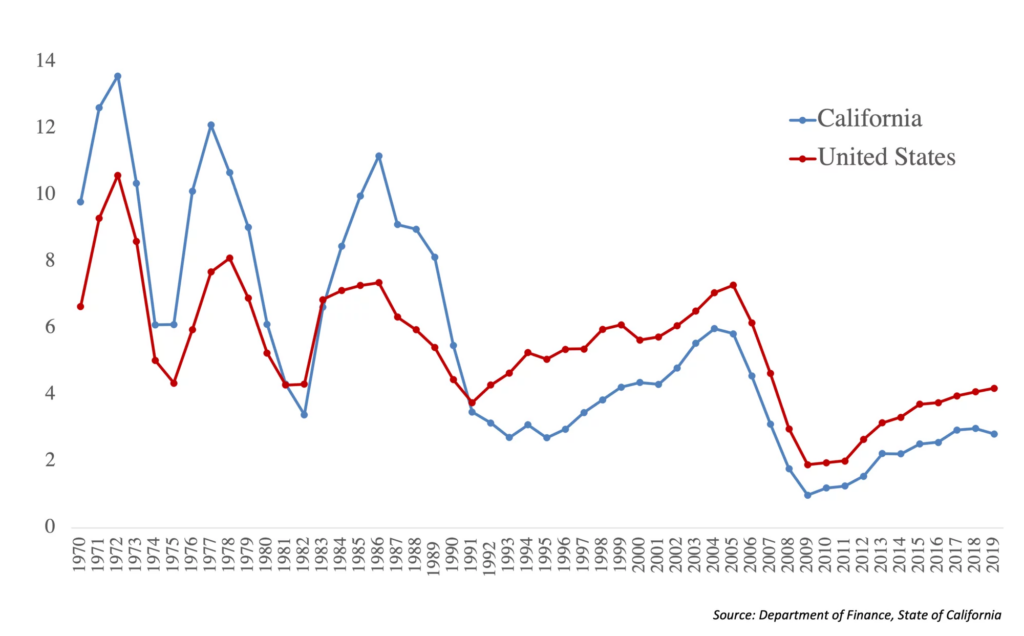
While the housing demand has surged, the supply has fallen short of the national average since 1991, as demonstrated in Figure 3. The supply shortage is exceptionally sharp in coastal cities. For example, San Francisco added 38,000 new jobs from 2016 to 2018 but built only 4,500 new housing units (McQuillan 2020). California ranks 49th among all U.S. states for housing units per capita (McKinsey Global Institute 2016).
Figure 3: Residential Building Permits, Per 1K Population
One key factor exacerbating the housing supply shortage is the single-family zoning and local opposition to housing, often embodied by the “not in my backyard,” or NIMBY, sentiment. Each additional growth control policy a community added was associated with a 3-5 percent increase in home prices (Taylor 2015; Rothwell 2019).
Another factor is the high costs and uncertainties in housing development related to lengthy entitlement processes, which include zoning changes, permit applications, standards variances, site plan reviews, design reviews, and environmental impact reviews (EIR) required by the California Environmental Quality Act (CEQA).
For projects that required an EIR, the average timelines for approvals were 43 months in Los Angeles and 77 months in Santa Monica (O’Neill, Gualco-Nelson, and Biber 2018). In recent years, some CEQA lawsuits tried to block infill housing (i.e., new housing on vacant, underused lots in an older neighborhood) and housing projects near transit lines. CEQA lawsuits can be filed anonymously and by parties attempting to advance an economic rather than environmental agenda, such as business competitors (Hernandez 2018; Hernandez et al. 2019).
Legislative efforts have been made in recent years to accelerate housing production, subdivide lots, and relax certain zoning restrictions to allow for more home building. Senate Bill 35 was signed into law in 2017, aiming to streamline the approval processes for multifamily housing development. Senate Bill 9 was ratified four years later, allowing many homeowners to build additional units on their property or subdivide their land into two lots. While this could help create more than 700,000 new homes that would otherwise not be market feasible, owner-occupancy requirements may mean that only a share of that potential will likely be developed (Metcalf et al. 2021). Despite the recent policy achievements, the housing supply shortage will persist in the near future.
A dearth of shelters
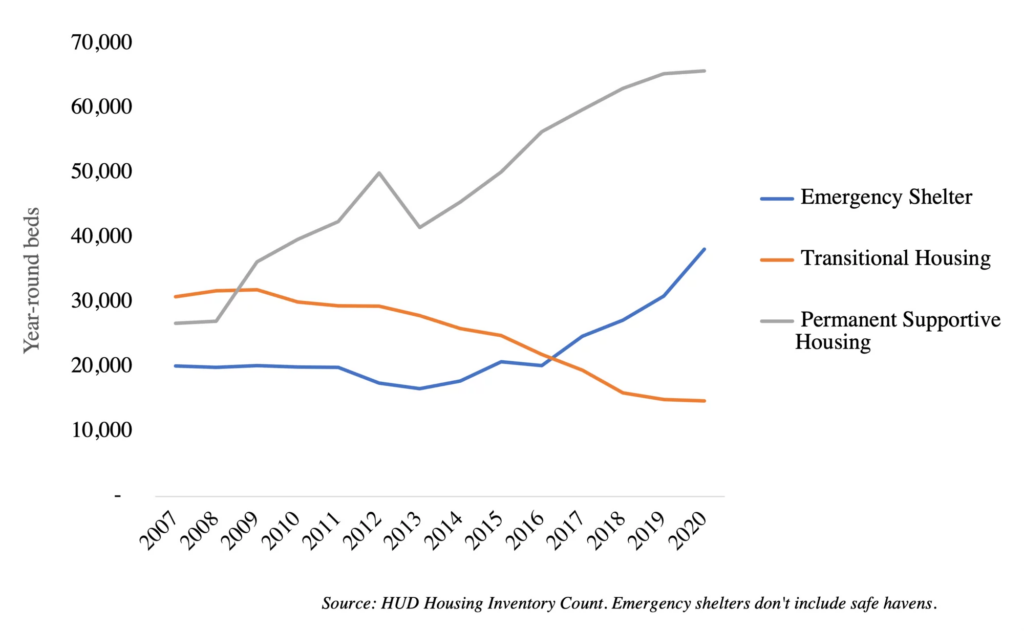
About 70 percent of the homeless in California are unsheltered, more than in any other state. A primary reason for the sizable unsheltered population is the low stock of emergency shelters and transitional housing. Between 2007 and 2020, while the total homeless population increased in California, the shelter capacity remained flat for a decade before rising again after 2017, and the bed counts at transitional housing facilities had a continuous decline.
Figure 4: Year-round beds in emergency shelters, transitional housing, and permanent supportive housing, California, 2007-2020
While the development of shelters has stagnated, there’s been a push for “Housing First” among many advocates and policymakers who believe permanent housing plus supportive services is the most important step to solving chronic homelessness.
Housing First is both an ideology and a practice developed in the 1990s that broke from the model of requiring homeless people to transition from emergency shelters to more permanent subsidized housing only when they met certain criteria around sobriety or treatment for mental illness.
The Housing First approach immediately provides homeless clients with an apartment and supportive services for drug addiction and/or mental illness (Tsemberis 2004). The supportive services are provided but participation is not required of the homeless clients.
Some benefits were attributed to Housing First, including higher housing stability, fewer emergency room visits, and improved medication adherence (Tsemberis, Gulcur, and Nakae 2004; Padgett, Henwood, and Tsemberis 2015; Aubry et al. 2016; Buchanan et al. 2009).
Meanwhile, Housing First showed no effects in reducing drug use, alcohol consumption, psychiatric symptoms, or enhancing the quality of life (Rosenheck et al. 2003; Mares, Greenberg, and Rosenheck 2007; Stergiopoulos et al. 2010).
Throughout the 2000s, Housing First received ample attention from academics, news media, and policymakers. But the policy carried unintended consequences when resources were diverted from shelters and other interim housing to building permanent housing projects.
For example, then-San Francisco Mayor Gavin Newsom presented a 10-year plan in 2004 that promised 3,000 new permanent supportive housing units in the following decade.
At the end of the decade, the city had been on track in creating permanent supportive housing. But city planners didn’t anticipate an influx of homeless people, for whom the original plan was unable to accommodate.
The shelter capacity was weakened as the plan “directed the City to move its focus away from traditional emergency shelters and toward shelters with 24-hour crisis clinics and sobering centers.” As a result, the city reduced 440 year-round emergency shelter beds between 2005 and 2014 while adding only 26 beds with some crisis or sobering management (City and County of San Francisco 2014).
Figure 5: San Francisco Built No New Shelters during the 10-Year-Plan Period
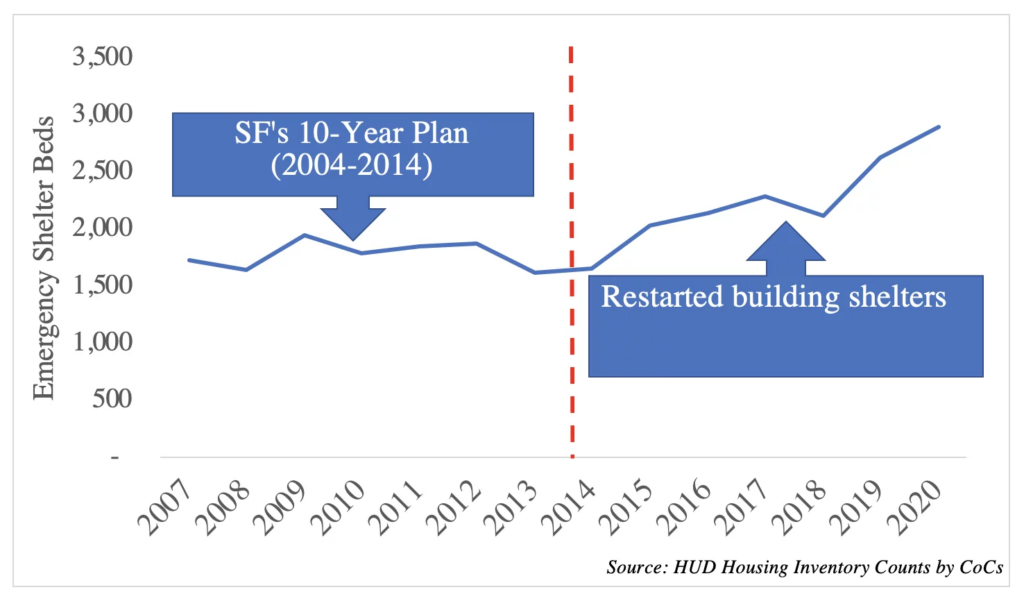
With a rising homeless population and a shrinking shelter capacity, San Francisco’s unsheltered homeless population doubled from about 2,655 to 5,180 between 2005 and 2019. After the 10-year plan ended in 2014, city planners began building shelters again, but it was too little too late.
Building permanent supportive housing was embraced with similar enthusiasm in Southern California. In 2016, Los Angeles voters approved Prop. HHH, which authorized city officials to issue up to $1.2 billion in bonds to reduce homelessness by developing and remodeling permanent supportive housing. According to a report by the L.A. Controller Ron Galperin, five years after the passing of the proposition, only 14 percent of promised projects had been completed, a total of 1,142 units. Development costs were high and continued to rise. In 2021, the average per-unit cost was almost $600,000. Some units are extremely expensive. Fourteen percent of the units exceeded $700,000, and at least one project is estimated to cost nearly $837,000 per unit.
Using permanent housing to solve homelessness met with the reality of California housing development: slow and expensive.
It takes about four years to complete an affordable housing project in the Bay Area, costing about $400,000 to $700,000 per unit, typically a studio, one-bed, or two-bed apartment (Bay Area Council Economic Institute 2021).
Cheaper, faster alternatives exist. For example, a bed costs about $43,000 in a shelter and $73,000 in a “tiny home” — compact housing units that can be quickly built (Bay Area Council Economic Institute 2021). While these options have disadvantages such as crowding and restrictive rules (e.g., no pets) and are less permanent or aesthetically appealing than long-term houses, policymakers need to weigh those shortcomings against the suffering of people sleeping on the street.
In states with sufficient housing stock and a small number of homeless people, Housing First can solve the “houseless” problem. Still, intensive care is needed if the root cause of an individual’s homelessness is mental illnesses, drug addiction, or alcohol abuse (Pearson 2007).
In contrast, in places with a housing shortage, such as coastal California, there is a long wait before permanent housing becomes available, which defies the original vision of Housing First to immediately provide an apartment (Tsemberis, Gulcur, and Nakae 2004). As cautioned in a JAMA paper, the high capital costs to develop permanent supportive housing in some localities can prohibit Housing First as a viable option (Kertesz and Weiner 2009).
In 2020, only one-third of California’s homeless moved into permanent housing, 47 percent were awaiting housing and still accessing services, and 16 percent were no longer engaging in services (San Jose Mayor’s Office 2021). While waiting for permanent housing, it’s imperative for homeless people to have a safe place to sleep. The longer people stay unsheltered, the more their mental and physical health deteriorates, making it harder for them to go back to the labor force, find housing, and regain financial stability.
Mental illness, drug addiction, and crime
Drug addiction and mental illness are consistent risk factors for homelessness (Tsai and Rosenheck 2015; Thompson et al. 2013; Yamamoto et al. 2019). Substance use can be both a cause and a result of homelessness (Johnson and Chamberlain 2008).
There are also differences in terminologies. In 2019, the Los Angeles Homeless Services Authority released a report showing 25 percent of the unsheltered homeless had a severe mental illness and 14 percent had a substance use disorder. Using the same survey data, the Los Angeles Times showed a much higher prevalence level: about 51 percent with mental illness and 46 percent with substance use disorder. The critical difference lies in the definition of mental health and drug addiction. The government’s estimates are lower because they only counted people with a permanent or long-term severe condition (LAHSA 2020).
Appendix Table A.1. contains estimates for the prevalence of mental illness and drug addiction among the homeless. The prevalence is particularly high among the chronically homeless, over 75 percent of whom have substance abuse or a severe mental illness (Kuhn and Culhane 1998; Poulin et al. 2010; Ellen Lockard Edens, Mares, and Rosenheck 2011). Powerful drugs such as P2P methamphetamine induce psychosis, the symptoms of which are sometimes confused with schizophrenia.
Several structural changes are related to the mental illness and drug addiction crisis seen among the unsheltered homeless population in California today.
Deinstitutionalization
The 1950s brought two key developments that affected homelessness. First, through books such as The Shame of the States by Albert Deutsch, the public gained insights into practices at many of those institutions, which were criticized as cruel and inhumane. In 1954, chlorpromazine (also known as “Thorazine”) was approved by the U.S. Food and Drug Administration as a new antipsychotic drug, which gave many people hope that mental health patients could live in the community with the help of medication.
In 1963, President Kennedy signed the Community Mental Health Act into law to provide federal funding for community-based mental health care, aiming at replacing institutional care with community care. At the same time, federal law generally prohibited states from using Medicaid funds to pay for non-elderly adults (i.e., age 21-64) in “institutions for mental disease” (IMDs).2 As state mental hospitals were considered IMDs and ineligible for Medicaid funds, states responded by closing down state mental hospitals (Geller 2000).
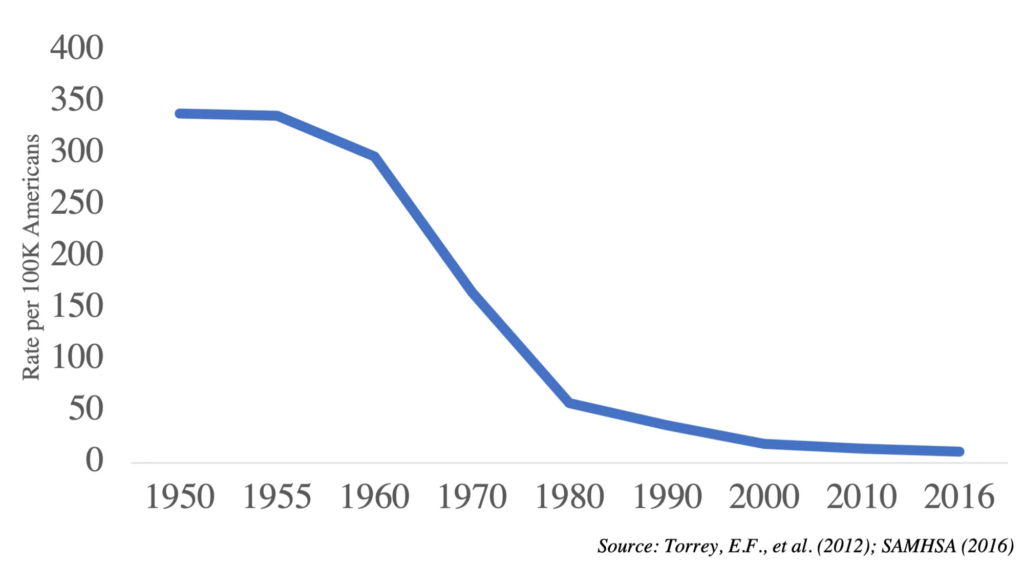
As a result of the nationwide deinstitutionalization, the number of mentally ill patients in public psychiatric hospitals plummeted from 558,239 in 1955 to 37,209 in 2016. As shown in Figure 6, the number of patients per 100,000 Americans decreased from 337 in 1955 to 11 in 2016 (Torrey et al. 2012; Treatment Advocacy Center 2016a; SAMHSA 2016).
However, the vision of providing care in the community didn’t materialize as was planned. The increase of beds in the community didn’t nearly make up for the loss of beds in public mental hospitals. Even if we add all other beds, including ones in private hospitals, general hospitals with psychiatric units, VA Medical Centers, and 24-hour residential treatment centers, the total beds throughout the country were about 170,000 in 2014, compared with over 550,000 in 1955 (SAMHSA 2016).
With the closing of state psychiatric hospitals and inadequate community-based care, streets, jails, and prisons have become the new asylum for many of the mentally ill.
Figure 6: Number of Inpatients in Public Mental Hospitals per 100K Americans
California was no exception amid the nationwide deinstitutionalization and has had a shortage of adult psychiatric beds. According to a RAND study (McBain et al. 2022), California is estimated to have a shortfall of 4,767 acute and sub-acute inpatient beds and 2,963 community residential beds. The magnitude of the state’s need for adult psychiatric beds is expected to grow over time.
Short of psychiatric inpatient beds, emergency room doctors often have little choice but to release mentally ill patients within a few days. Some patients may be referred to a county or private agency for help. But the time and effort it takes to access those services can be a barrier for many.
In recent years, there have been policy efforts to allow managed care organizations (MCOs) to receive Medicaid reimbursement for acute psychiatric care. But that care extends to only 15 days per month (Treatment Advocacy Center 2016b).
Realignment and Proposition 47
In the past decade, California began enacting laws to reform the criminal justice system and reduce populations in the state’s overcrowded prisons. But some advocates and policymakers now recognize that legislation may be having unintended consequences for some homeless people.
With the state’s prison population swollen to nearly 174,000 inmates — 200 percent of capacity — the California Public Safety Realignment Act (AB 109) was passed in 2011. The law meant low-level offenders would now receive sentences in county jail or non-custodial mandatory supervision rather than being sentenced to state prison.
Three years later, voters passed Proposition 47, which recategorized some nonviolent offenses from felonies to misdemeanors. This included burglary and theft under $950 and possession of controlled substances including cocaine, heroin, and methamphetamine (Proposition 47 FAQ). In 2021, S.B. 73 was signed into law, which further ended mandatory minimum sentences by giving judges discretion to grant probation instead of jail time for nonviolent drug crimes.
AB 109 and Proposition 47 reduced prison overcrowding, arrests, felony conviction, and long incarcerations (Bird et al. 2016; Petersilia et al. 2014; Mooney et al. 2019). But the laws also reduced the number of people going through drug courts — and being able to access services to help stabilize sobriety.
Overseen by a judge, a drug court seeks to harness the coercive power of the criminal justice system to persuade drug offenders to receive treatment (U.S. Department of Health and Human Services HHS 2016). If they pass the drug treatment program, their charges are dismissed. Studies have shown the effectiveness of drug courts on increasing treatment completion, reducing recidivism, incarceration, and subsequent drug use (Gottfredson, Najaka, and Kearley 2003; Wilson, Mitchell, and MacKenzie 2006; Sevigny, Fuleihan, and Ferdik 2013; Belenko, Patapis, and French 2005).
After the passing of Proposition 47, many of those already in the drug court system began dropping out of mental health and substance use disorder treatment. Moreover, the number of individuals referred to treatment by the criminal justice system also decreased (Hunter et al. 2017).
Homeless persons addicted to drugs face high barriers to access treatment in the community. Such barriers include long waiting lists for treatment programs that accept Medi-Cal, logistic constraints like the lack of a phone (to call in order to enroll), transportation, and documentation, and no help in accessing treatment (Brubaker et al. 2013). The new laws may have taken away an effective channel through which some homeless would have been able to access and complete drug treatment.
Policy Considerations
Homelessness in California is complex, and the diverse causes and trajectories of homelessness suggest the solutions are also diverse. Policymakers should consider a combination of strategies that address the housing shortage and costs issues and those that tackle the mental health and drug addiction crisis.
Housing development
- Streamline and expedite the approval process for new housing projects.
- Simplify funding applications for affordable housing projects.
- Expand permissible residential development on commercial property (Metcalf et al. 2021).
- Expand the use of CEQA exemptions.
- Amend CEQA to eliminate the automatic right of appeal for meritless cases and to prevent ambushes in which claimants raise issues too late (Kolkey 2019).
Shelters, interim housing, and alternative housing options
- Expand shelter capacity, including congregate and non-congregate shelters.
- Improve the quality and safety of congregate shelters and eliminate unnecessary rules such as restrictions on pets.
- When there are shelter spaces, the “right-to-shelter” should be enforced. Other rules such as no public defecation and public urination should be enforced to address the quality-of-life issues.
- Increase the development of innovative, cost-effective housing, such as tiny homes and modular homes.
- Promote shared-housing and consider reducing the implicit tax on housing sharing (He, O’Flaherty, and Rosenheck 2010; Ellen and O’Flaherty 2007).
Permanent supportive housing
- Conduct in-depth research on the long-term outcomes of permanent supportive housing (PSH), to understand the effects of PSH on labor force participation, drug use, and psychiatric symptoms.
- County governments conduct site inspections on whether the PSHs have a sufficient staff-to-client ratio and whether homeless clients living in PSHs can receive timely, adequate treatments for their mental illness and drug addiction.
Mental health treatment
- Increase psychiatric beds at the acute, sub-acute, and community residential levels (to prevent mental health patients being released prematurely).
- Lower the barriers for the homeless with a mental illness to seek treatment (e.g., shorten the wait time for intakes to accommodate the needs of mental health patients).
- CARE (Community Assistance, Recovery & Empowerment) Court, a new framework that’s still unfolding, has the potential to provide useful tools to help those with severe mental health and substance abuse problems.
- For individuals lacking insight into their illness or unable to access community treatment voluntarily, Laura’s Law should be invoked to compel them to receive treatment detailed in the assisted outpatient treatment (AOT) order.
- Use Lanterman-Petris-Short (LPS) conservatorships for adults with serious mental health illness and gravely disabled (i.e., cannot take care of basic, personal needs for food, clothing, or shelter).
Drug addiction
- Build the infrastructure for addiction treatment inside hospitals to broaden the access to addiction treatment.
- Lower the barriers for homeless drug addicts to seek treatments (e.g., not requiring phone calls to be the first step of enrollment since many homeless have no easy access to phones).
- Increase the number of treatment facilities that accept Medi-Cal, which covers most homeless persons.
- Increase the number of treatment facilities with detox beds and residential care to reduce wait time and achieve “treatment on demand.”
- Make appropriate use of drug courts to incentivize people into receiving and completing addiction treatments.
- Improve accountability by enforcing the law on petty crimes, which are used by some homeless persons to sustain drug use habits.
Jialu Streeter a Research Scholar and the Director of Partnerships at the SIEPR. Her research primarily focuses on the economics of aging, retirement security, and financial security and mental wellbeing of older adults.
Table A.1.: The prevalence of mental illness and substance use among the homeless population.
| Research | Mental illness | Drug abuse | Alcohol abuse | Notes |
|---|---|---|---|---|
| (1) For the Chronically Homeless | ||||
| Kuhn and Culhane (1998) | 75 percent had substance abuse or severe mental illness | 7196 chronically homeless in Philadelphia; treatment matched disabilities | ||
| Poulin, Maguire, Metraux, and Culhane (2010) | 30 percent (diagnosis of serious mental illness) | 48 percent (records of substance abuse treatment) | 2,703 chronically homeless persons in Philadelphia | |
| Edens, Mares, and Rosenheck (2011) | 76 percent | 52 percent | 52 percent | 714 chronically homeless in the 11-site Collaborative Initiative on Chronic Homelessness |
| (2) Other Homelessness Samples | ||||
| Robertson, Zlotnick, and Westerfelt (1997) | 52 percent | 53 percent | Countywide probability sample of homeless adults in Alameda County, California (n=564) | |
| Burt and Aron (2001) | 57 percent | 58 percent | 62 percent | 2938 homeless individuals in the National Survey of Homeless Assistance Providers and Clients (NSHAPC) |
| Fountain and Howes (2004) | 83 percent | 389 homeless persons were interviewed in Britain | ||
| Johnson and Chamberlain (2008) | 43 percent | 4291 homeless individuals gathered at two service agencies working with people at risk of homelessness and those who are actually homeless in Melbourne, to be representative of the inner city homeless | ||
| Edens, Kasprow, Tsai, and Rosenheck (2011) | 48 percent | 45 percent | 109,056 homeless veterans who used V.A. mental health services. | |
| Montgomery, et al. (2016) | 54 percent (ever been treated for mental health problems) | 70 percent (substance abuse) | 17 percent (drank alcohol every day in the past month) | 25489 homeless persons (13,761 unsheltered + 11,728 sheltered) from 62 communities between 2008 and 2014, who responded to the 100,000 Homes Vulnerability Index survey in the U.S. |
| Bymaster, et al. (2017) | 80 percent | 88 percent | 59 percent | 125 homeless people who were obtaining health care at two clinic sites of the Santa Clara County Homeless Program (08/2013-05/2014) |
| Bowie and Lawson (2018) | 45 percent | 79 percent (substance abuse) | 46 homeless individuals encountered at a drop-in day center, a temporary winter overnight shelter, or on the street | |
| (3) Based on Point-in-Time Data | ||||
| L.A. Homeless Services Authority (2019) | 25 percent (serious, long-term conditions) | 14 percent (serious, long-term conditions) | L.A. continuum of care (CoC) Point-in-Time estimates | |
| L.A. Homeless Services Authority (2020) | 25 percent (serious, long-term conditions) | 27 percent (serious, long-term conditions) | L.A. continuum of care (CoC) point-in-time estimates | |
| Evans, et al. (2019) | 20 percent (serious, long-term conditions) | 16 percent (serious, long-term conditions) | 2017 Point-in-Time estimates from different continuums of care (CoCs) | |
Note: Substance abuse can include the abuse of drugs and alcohol. The estimates based on Point-in-Time data tend to be lower because (i) the data focus on serious conditions that last long term or permanently and (ii) the point-in-time data sample includes all homeless, sheltered and unsheltered, individuals with and without children
Footnotes
[1] Chronically homeless is defined as a person who is homeless for at least 1 year or 4+ separate occasions in the last 3 years and has a substance use disorder, serious mental illness, developmental disability, PTSD, cognitive impairments from brain injury, or chronic physical illness or disability (HUD 2009). In California, chronically homeless account for one-third of all homeless.
[2] The definition of IMDs has been modified many times. Between 1966 and 1988, a facility was deemed an IMD if it was licensed as a psychiatric facility, accredited as a psychiatric facility, or under the jurisdiction of the state’s mental health authority. After 1988, a facility would be classified as an IMD if it had more than 16 psychiatric treatment beds.
References
ABC. 2021. “ ‘California Dreaming’ Five-Part Series.” ABC7 Los Angeles. February 9, 2021.
Aubry, Tim, Paula Goering, Scott Veldhuizen, Carol E. Adair, Jimmy Bourque, Jino Distasio, Eric Latimer, et al. 2016. “A Multiple-City RCT of Housing First With Assertive Community Treatment for Homeless Canadians With Serious Mental Illness.” Psychiatric Services 67 (3): 275–81.
Bay Area Council Economic Institute. 2021. “Bay Area Homelessness: New Urgency, New Solutions.”
Belenko, Steven, Nicholas Patapis, and Michael French. 2005. “Economic Benefits of Drug Treatment: A Critical Review of the Evidence for Policy Makers | Office of Justice Programs.” U.S. DOJ Office of Justice Programs.
Bird, Mia, Sonya Tafoya, Ryken Grattet, and Viet Nguyen. 2016. “How Has Proposition 47 Affected California’s Jail Population?” 20.
Bowie, Bonnie H., and Lauren Valk Lawson. 2018. “Using the Vulnerability Index® to Assess the Health Needs of a Homeless Community.” Journal of Community Health Nursing 35 (4): 189–95.
Brubaker, Michael D., Ellen A. Amatea, Edil Torres-Rivera, M. David Miller, and Laura Nabors. 2013. “Barriers and Supports to Substance Abuse Service Use Among Homeless Adults.” Journal of Addictions & Offender Counseling 34 (2): 81–98.
Buchanan, David, Romina Kee, Laura S. Sadowski, and Diana Garcia. 2009. “The Health Impact of Supportive Housing for HIV-Positive Homeless Patients: A Randomized Controlled Trial.” American Journal of Public Health 99 (S3): S675–80.
Burt, Martha R., and Laudan Aron. 2001. Helping America’s Homeless. The Urban Institute Press.
Bymaster, Angela, Joyce Chung, Andrea Banke, Hee Jae Choi, and Chelsea Laird. 2017. “A Pediatric Profile of a Homeless Patient in San Jose, California.” Journal of Health Care for the Poor and Underserved 28 (1): 582–95.
CA Government, Metropolitan Transportation Comission. 2019. “Which Industries Are Creating or Losing Jobs?” Vital Signs.
City and County of San Francisco. 2014. “San Francisco’s Ten-Year Plan to End Chronic Homelessness: Anniversary Report Covering 2004 to 2014.” San Francisco Human Services Agency, City and County of San Francisco.
Edens, Ellen L., Wes Kasprow, Jack Tsai, and Robert A. Rosenheck. 2011. “Association of Substance Use and VA Service-Connected Disability Benefits with Risk of Homelessness among Veterans.” The American Journal on Addictions 20 (5): 412–19.
Edens, Ellen Lockard, Alvin S. Mares, and Robert A. Rosenheck. 2011. “Chronically Homeless Women Report High Rates of Substance Use Problems Equivalent to Chronically Homeless Men.” Women’s Health Issues 21 (5): 383–89.
Ellen, Ingrid Gould, and Brendan O’Flaherty. 2007. “Social Programs and Household Size: Evidence from New York City.” Population Research and Policy Review 26 (4): 387–409.
Evans, William N., David C. Philips, and Krista J. Ruffini. 2019. “Reducing and Preventing Homelessness: A Review of the Evidence and Charting a Research Agenda.” Working Paper 26232. Working Paper Series. National Bureau of Economic Research.
Fountain, Jane, and Samantha Howes. 2004. Home and Dry? Homelessness and Substance Use. London: National Addiction Centre.
Geller, Jeffrey L. 2000. “Excluding Institutions for Mental Diseases From Federal Reimbursement for Services: Strategy or Tragedy?” Psychiatric Services 51 (11): 1397–1403.
Gottfredson, Denise C., Stacy S. Najaka, and Brook Kearley. 2003. “Effectiveness of Drug Treatment Courts: Evidence from a Randomized Trial*.” Criminology & Public Policy 2 (2): 171–96.
Har, Janie. 2021. “Audit: California Should Track Homeless Spending, Set Policy.” AP News, 2021.
He, Yinghua, Brendan O’Flaherty, and Robert A. Rosenheck. 2010. “Is Shared Housing a Way to Reduce Homelessness? The Effect of Household Arrangements on Formerly Homeless People.” Journal of Housing Economics 19 (1): 1–12.
Hernandez, Jennifer. 2018. “California Environmental Quality Act Lawsuits and California’s Housing Crisis.” Hastings Environmental Law Journal 24 (1): 52.
Hernandez, Jennifer, David Friedman, Stephanie DeHerrera, and Holland & Knight. 2019. “In the Name of the Environment: Litigation Abuse Under CEQA.”
Hunter, Sarah B., Lois M. Davis, Rosanna Smart, and Susan Turner. 2017. “Impact of Proposition 47 on Los Angeles County Operations and Budget.” RAND Corporation.
Johnson, Guy, and Chris Chamberlain. 2008. “Homelessness and Substance Abuse: Which Comes First?” Australian Social Work 61 (4): 342–56.
Kertesz, Stefan G., and Saul J. Weiner. 2009. “Housing the Chronically Homeless: High Hopes, Complex Realities.” JAMA 301 (17): 1822–24.
Kolkey, Daniel. 2019. “CEQA: How to Mend It since You Can’t End It.” Orange County Register (blog). 2019.
Kuhn, R., and D. P. Culhane. 1998. “Applying Cluster Analysis to Test a Typology of Homelessness by Pattern of Shelter Utilization: Results from the Analysis of Administrative Data.” American Journal of Community Psychology 26 (2): 207–32.
LAHSA. 2020. “2020 Greater Los Angeles Homeless Count Demographic Survey Packet.” 2020.
Mares, Alvin, Greg Greenberg, and Robert Rosenheck. 2007. “HUD/HHS/VA Collaborative Initiative to Help End Chronic Homelessness: Is System Integration Associated with Client Outcomes?” U.S. Department of Health and Human Services.
McBain, Ryan K., Jonathan H. Cantor, Nicole K. Eberhart, Shreya S. Huilgol, and Ingrid Estrada-Darley. 2022. “Adult Psychiatric Bed Capacity, Need, and Shortage Estimates in California—2021.” RAND Corporation.
McQuillan, Lawrence J. 2020. “How to Restore the California Dream: Removing Obstacles to Fast and Affordable Housing Development.” Independent Institute.
McKinsey Global Institute. 2016. “Closing California’s Housing Gap.” McKinsey & Company.
Metcalf, Ben, David Garcia, Ian Carlton, Mapcraft Labs, and Kate Macfarlane. 2021. “Assessing the Viability of New Housing Supply Under California’s Senate Bill 9.” Terner Center for Housing Innovation – UC Berkeley, 21.
Montgomery, Ann Elizabeth, Dorota Szymkowiak, Jessica Marcus, Paul Howard, and Dennis P. Culhane. 2016. “Homelessness, Unsheltered Status, and Risk Factors for Mortality.” Public Health Reports 131 (6): 765–72.
Mooney, Alyssa C., Torsten B. Neilands, Eric Giannella, Meghan D. Morris, Jacqueline Tulsky, and M. Maria Glymour. 2019. “Effects of a Voter Initiative on Disparities in Punishment Severity for Drug Offenses across California Counties.” Social Science & Medicine 230 (June): 9–19.
O’Neill, Moira, Guilia Gualco-Nelson, and Eric Biber. 2018. “Examining the Local Land Use Entitlement Process in California to Inform Policy and Process.” Berkeley Center for Law, Energy & the Environment.
Padgett, Deborah K., Benjamin F. Henwood, and Sam J. Tsemberis. 2015. “Housing First Gets Its Evidence Base and Momentum Builds.” In Housing First. Oxford University Press.
Petersilia, Joan, Sara Abarbanel, John S Butler, Mark Feldman, Mariam Hinds, Kevin E Jason, Corinne Keel, Matt J Owens, and Camden Vilkin. 2014. “Voices from the Field: How California Stakeholders View Public Safety Realignment.” SSRN Electronic Journal.
Poulin, Stephen R., Marcella Maguire, Stephen Metraux, and Dennis P. Culhane. 2010. “Service Use and Costs for Persons Experiencing Chronic Homelessness in Philadelphia: A Population-Based Study.” Psychiatric Services 61 (11): 1093–98.
Robertson, M. J., C. Zlotnick, and A. Westerfelt. 1997. “Drug Use Disorders and Treatment Contact among Homeless Adults in Alameda County, California.” American Journal of Public Health 87 (2): 221–28.
Rosenheck, Robert, Wesley Kasprow, Linda Frisman, and Wen Liu-Mares. 2003. “Cost-Effectiveness of Supported Housing for Homeless Persons With Mental Illness.” Archives of General Psychiatry 60 (9): 940–51.
Rothwell, Jonathan. 2019. “Land Use Politics, Housing Costs, and Segregation in California Cities.” UC Berkeley Terner Center for Housing.
SAMHSA. 2016. “National Mental Health Services Survey (N-MHSS): 2016, Data On Mental Health Treatment Facilities | CBHSQ Data.”
San Diego County. n.d. “Proposition 47 FAQ.” San Diego County Government, Office of the Public Defender. Accessed May 10, 2022.
San Jose Mayor’s Office. 2021. “California’s Big City Mayors Boldly Ask State Leaders for Record Level Funds to End Homelessness | Office of the Mayor – Latest News | City of San Jose.” City of San Jose. 2021.
Sevigny, Eric L., Brian K. Fuleihan, and Frank V. Ferdik. 2013. “Do Drug Courts Reduce the Use of Incarceration?: A Meta-Analysis.” Journal of Criminal Justice 41 (6): 416–25.
Stergiopoulos, Vicky, Carolyn S. Dewa, Gordon Tanner, Nancy Chau, Mike Pett, and Jo Lynn Connelly. 2010. “Addressing the Needs of the Street Homeless.” International Journal of Mental Health 39 (1): 3–15.
Taylor, Mac. 2015. “California’s High Housing Costs – Causes and Consequences.” Legislative Analyst’s Office (LAO).
Thompson, Ronald G., Melanie M. Wall, Eliana Greenstein, Bridget F. Grant, and Deborah S. Hasin. 2013. “Substance-Use Disorders and Poverty as Prospective Predictors of First-Time Homelessness in the United States.” American Journal of Public Health 103 (S2): S282–88.
Torrey, Fuller, Doris Fuller, Jeffrey Geller, Carla Jacobs, and Kristina Ragosta. 2012. “No Room at the Inn: Trends and Consequences of Closing Public Psychiatric Hospitals 2005-2010.” Treatment Advocacy Center.
Treatment Advocacy Center. 2016a. “Serious Mental Illness Prevalence in Jails and Prisons.”
———. 2016b. “The Medicaid IMD Exclusion and Mental Illness Discriminiation.”
Tsai, Jack, and Robert A. Rosenheck. 2015. “Risk Factors for Homelessness among US Veterans.” Epidemiologic Reviews 37: 177–95.
Tsemberis, Sam, Leyla Gulcur, and Maria Nakae. 2004. “Housing First, Consumer Choice, and Harm Reduction for Homeless Individuals With a Dual Diagnosis.” American Journal of Public Health 94 (4): 651–56.
U.S. Department of Health and Human Services (HHS). 2016. “EARLY INTERVENTION, TREATMENT, AND MANAGEMENT OF SUBSTANCE USE DISORDERS.” In Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, D.C.: U.S. Department of Health and Human Services.
Wilson, David B., Ojmarrh Mitchell, and Doris L. MacKenzie. 2006. “A Systematic Review of Drug Court Effects on Recidivism.” Journal of Experimental Criminology 2 (4): 459–87.
Yamamoto, Ayae, Jack Needleman, Lillian Gelberg, Gerald Kominski, Steven Shoptaw, and Yusuke Tsugawa. 2019. “Association between Homelessness and Opioid Overdose and Opioid-Related Hospital Admissions/Emergency Department Visits.” Social Science & Medicine 242 (December): 112585.